Gardasil (HPV Vaccine) is a complicated decision for clinicians and parents.
Moisturizers Up Skin Cancer in Mice. So what?
August 15, 2008Researcher on Abortion-Depression Link Says APA Report Ignores Best Studies
August 15, 2008The Los Angeles Times is reporting that although “most medical organizations strongly advocate using” Gardasil, “the human papilloma virus (HPV) vaccine that may prevent cervical cancer,” a number of clinicians and parents “are asking whether the vaccine’s benefits really outweigh its costs.”
My Take?
I agree with those who told the Times “they aren’t convinced that the expensive shots offer any more protection than preventive measures already available — principally, regular screening via the Pap smear test.”
And, it’s reasonable to think that “blanket immunizations of the nation’s adolescents could backfire by lulling them into a false sense of security that leads them to neglect regular screening.”
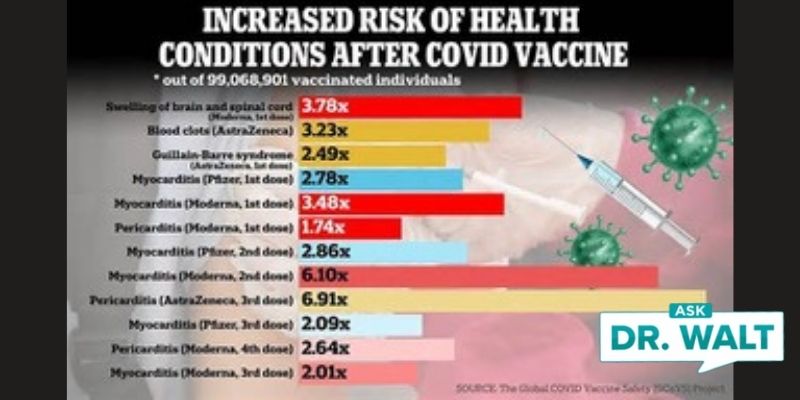
Moreover, as I’ve previously reported in this blog, in June, Judicial Watch “obtained records from the” Food and Drug Administration’s Vaccine Adverse Event Reporting System, and found that some women who had been inoculated, experienced “serious events — such as seizures, spontaneous abortions, and even deaths.”
Still, Laurie E. Markowitz, M.D., of the Centers for Disease Control and Prevention, maintains that the “deaths, and all the other serious events, could have happened in the absence of the vaccine.” She “remains convinced the vaccine is safe.”
Maybe? But is it as effective as they claim? And, is it cost-effective?
I believe these issues are still open to debate. Maybe they should have been answered before medical organizations began recommending each family of each teen girl spend up to $400 on this vaccine.
Remember, Gardasil protects only against the HPV strains linked most strongly to cervical cancer.
“We don’t know if it will make a difference in the ultimate rates of cancer,” says Abby Lippman, an epidemiologist at McGill University in Montreal who has researched the HPV vaccine. “The jury is still out on how much benefit we’re actually going to get with this vaccine.”
The American College of Obstetricians and Gynecologists recommended that girls get the required series of three doses (given over a six-month period) at age 9 or older; the American Academy of Pediatrics and the Centers for Disease Control and Prevention recommended the same, with a starting age of 11 or later. (Because HPV is normally spread by intimate contact, the vaccine is considered most effective when given before the beginning of sexual activity. It will not eradicate HPV if someone is already infected.)
Since 2006, about 8 million females in the U.S. have received at least one shot of Gardasil, according to the vaccine’s maker, Merck & Co. of Whitehouse Station, N.J., which based these estimates on data from government and private insurers. Of the 100 known strains of HPV, about 30 cause cancer or genital warts.
Two strains — HPV-16 and HPV-18 — are responsible for 70% of cervical cancers.
Pre-market studies showed that the vaccine is 90% to 100% effective in thwarting the transmission of these two strains and two others, which are linked to 90% of genital warts.
But, most of the women on whom the vaccine was tested were older.
And, the vaccine is very expensive. It costs $360 for the series of three shots, and administrative fees can add $100 or more.
Though insurance companies sometimes cover costs, the overall expense for vaccinating the nations’ teenagers could run into billions, a bill that will affect taxpayers as the shots are given to recipients of government health programs and health insurance premiums rise.
The price simply may not be worth it, says Dr. Karen Smith-McCune, an obstetrician and gynecologist at the UC San Francisco School of Medicine interviewed by the Times.
Because it takes years for cervical cancer to develop, it is easily preventable as long as HPV infection is detected early.
Though the cancer is common in developing countries and kills more than 280,000 women worldwide every year, it is much less of a health threat in the U.S., she says, where 11,000 women are diagnosed with the disease annually, and about 3,700 will die of it.
The comparatively low U.S. incidence of cervical cancer is due to one of the public health system’s triumphs: widespread use of Pap smears, which detect abnormal cervical cells so they can be removed before they turn into cancers.
Adoption of the Pap test caused a reduction of cervical cancer rates by 74% between 1955 and 1992, according to the American Cancer Society. Rates continue to drop by 4% each year.
Smith-McCune and other critics of Gardasil also note that up to 90% of HPV infections in adolescents clear up on their own — meaning that cervical cancer will not develop even in most women infected with the most aggressive type of HPV.
In other words, a woman’s risk of developing cervical cancer is already extremely low, and the immune system normally makes short work of HPV without outside help.
Even if women get the vaccine, they still need to continue annual Pap screenings because they could contract other cancer-causing HPV strains that the vaccine does not fight.
“The crux of it is that we know how to prevent cervical cancer,” Smith-McCune says. “One of the key questions is whether this huge outlay of money for the vaccine is a better strategy than reaching out to the women who aren’t getting Pap tests and follow-ups.”
The Times correctly points out, “It is not yet proven that Gardasil actually prevents cervical cancer, which can take a decade to develop after HPV infection, because tests of the vaccine before the FDA greenlighted it didn’t run long enough to prove that conclusively.”
“Even though it guards against two HPV strains, the other HPV types need to be taken into account,” Smith-McCune says. “It will take a long time before we know the true efficacy of the vaccine.”
Even doctors who helped devise the vaccine point out that Pap screening may be more effective in cutting cervical cancer rates.
“If we vaccinate every single 12-year-old, it should reduce by half the number of cervical cancers in the next 35 years,” says Dr. Diane Harper, director of the Gynecologic Cancer Prevention Research Group at Dartmouth Medical School in Hanover, N.H., and a lead researcher in the development of the HPV vaccine. “With Pap screening, we’ve reduced it by nearly 75%.”
Then there is the issue of side effects. When the vaccine was tested in more than 11,000 females age 9 to 26 before its FDA approval, no serious ones emerged, though some subjects felt soreness at the injection site and, in rare instances, fainted after the shot.
But an analysis released June 30 by the Washington, D.C.-based public interest group Judicial Watch raised some red flags.
According to the Times, “Judicial Watch obtained records from the FDA’s Vaccine Adverse Event Reporting System (VAERS), a voluntary system used by doctors, patients and drug companies to report side effects with vaccines to the federal agency.
“The report revealed that since the vaccine’s 2006 approval, when girls began getting it, nearly 9,000 had bad health events after receiving Gardasil.
“The incidents included 10 miscarriages, 78 severe outbreaks of genital warts and six cases of Guillain-Barré syndrome, an autoimmune disorder that can result in paralysis. There were also 18 reported deaths.
Since the FDA’s VAERS is known to catch perhaps 10% of adverse events at best, according to a 2004 report in the New England Journal of Medicine by the FDA, the actual numbers may be far higher.
It is difficult to prove whether the vaccine was the culprit behind these side effects — just because two events happen, it does not mean that one caused the other, says Dr. Laurie E. Markowitz, an epidemiologist at the CDC who has had her own daughter vaccinated.
The deaths, and all the other serious events, could have happened in the absence of the vaccine, she says.
Markowitz remains convinced the vaccine is safe. “The CDC and the FDA checked out these reports very carefully,” she says. “And we’ve done calculations for the number of cases reported and the number of cases that you’d find in the general population, and we have not found an increase.”
Given these caveats, should girls be getting the shots?
Most major medical groups still think Gardasil should be part of routine immunizations for 11- and 12-year-old girls.
There is more than the matter of cancer prevention, says Dr. Joseph A. Bocchini, chief of pediatric infectious disease at Louisiana State University Health Sciences Center in Shreveport and chairman of the American Academy of Pediatrics committee on infectious diseases.
The vaccine could spare hundreds of thousands of women from the psychological trauma and physical pain of a cycle of follow-up tests when they have an abnormal Pap test result and the treatments for pre-cancerous lesions that can cause infertility.
“You can actually prevent these infections and the cervical abnormalities that require more invasive interventions,” he says.
But, “whether the shots should be mandatory — a step that has been considered by Texas, Michigan and Virginia — is another issue.”
“This decision should be up to parents, and mandates are silly,” says Harper of Dartmouth.
“While the vaccine will improve the health of American women, its real benefit is in the developing world. And no matter what, Pap screening shouldn’t be neglected. That’s still our best safety net.”
My recommendations? Avoid routine use of the vaccine. Emphasize sexual purity until marriage. Utilize annual pap smears after the onset of sexual activity.
These recommendations appear to me to have the most evidence supporting them.